In terms of pure biology, the twenties are an ideal time for a woman to have a child; the body is in an ideal state for it. But for some women, though the body may be ready, the mind is not. Perhaps you are pursuing a career that doesn’t leave time for child rearing and are waiting until your thirties, which certainly is a popular option these days.
If so, you may be looking for a way to prevent pregnancy. The more we understand our bodies and how they work, the better choices we can make regarding our health. This is particularly true when it comes to contraception.
Since men usually play a passive role when it comes to contraception, women have had to carry the burden of responsibility for birth control. So I think that the choice of birth control method is one that a woman needs to make on her own.
That said, I think it’s important for couples to talk about their contraception choices, and men should be a little more sensitive to everything that women have to do to avoid pregnancy. The choice of contraceptive methods has never been greater than it is today, but, as always, that choice should be based on the woman’s health, the frequency of sexual activity, the number of sexual partners, and the desire to have children in the future. Each of the various methods available involves some risks that must be considered.
Condoms The simplest and most obvious type of birth control is the barrier method, and the most popular type of barrier method for birth control is the latex or polyurethane condom, which exists for both men and women. The condom works by preventing the sperm from reaching the egg. Condoms will fail 11 times out of 100 and may cause latex allergy, irritation and vaginitis. On the other hand, condoms happen to be one of the best methods of preventing sexually transmitted diseases such as chlamydia, syphilis, gonorrhea, HIV and hepatitis.
Diaphragm Another type of barrier method, the diaphragm is a dome-shaped rubber device that a woman places inside the vagina, usually accompanied with a spermicidal cream, which kills the sperm. The diaphragm will fail 17 times out of 100 and counts among its side effects irritation, discomfort, urinary tract infection, and, in rare cases, toxic shock syndrome, especially when the diaphragm is not removed.
Cervical Cap Another barrier method is the cervical cap, a diaphragm-like device. The cap is placed inside the cervix by a gynecologist, often with great difficulty. Its side effects and faiure rates are similar to those of the diaphragm.
Sponge The sponge is a disk-shaped polyurethane device that is easily inserted at the time of intercourse and contains a spermicidal cream called nonoxynol-9. It has a good pregnancy prevention rate, failing only 14 times in 100.
Spermicide Some women use spermicide, nonoxynol-9, alone, in foam, jelly or suppository form. Spermicides sometimes cause irritations and allergies, and they have a very poor efficacy rate, failing 50 out of 100 times.
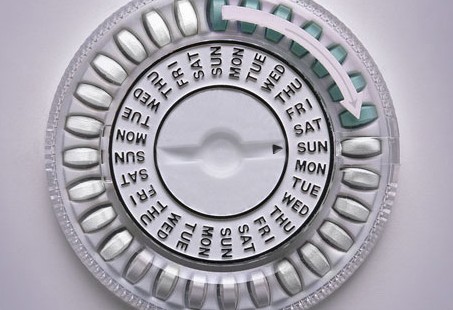
Oral Contraceptive Pill The “Pill” is probably the most popular method of birth control, probably because it’s easy to use and very effective. First introduced in the 1960’s, the Pill is a combination of estrogen and progestin hormones that essentially tell the body not to ovulate or release an egg from the ovaries. The Pill today contains very small quantities of both estrogen and progesterone, and it’s taken on a daily basis so that the body doesn’t get exposed to excessive amounts of hormones at one time. The Pill is very effective, with only two failures in 100. The problem is that the Pill does not prevent sexually transmitted diseases, and it can cause menstrual irregularities and stroke. The standard Pill is not recommended for women who are breastfeeding, though it is safe to take a progestin-only birth control pill while breast-feeding.
You have no doubt heard stories about a possible link between birth control pills and breast cancer. Whether or not this link is real is difficult to determine, however, since the results from various studies are conflicting. Yes, the more hormones you put into your body, the greater your risk of getting breast cancer. But if you’re on birth control pills for short periods of time, your risks are minimal. Even if you’re on the Pill for more than 10 years, your risk of breast cancer may increase, but that doesn’t necessarily mean you’ll get it. The birth control pills on the market today contain a lower dose of hormones than they did previously, so Pill users of today face a somewhat lower risk of breast cancer than Pill users of decades ago. Also, girls who start their periods when they’re really young and stop them when they’re really old are more at risk of breat cancer. Many factors come into play when talking about breast cancer. The best we can say right now about a link between birth control pills and breast cancer is….maybe.
Hormone Patch Requiring even less attention than the Pill is the hormone patch, Ortho Evra. The patch is worn on the abdomen or thigh, where progestin and estrogen are released and then absorbed by the skin. The problem with the patch is that it has been linked to high hormone levels and significant reports of strokes in young women. Just like with the Pill, anyone who has a family history of stroke, is a smoker, or is known to have a heart disorder should probably not use these types of devices.
Contraceptive Ring Another hormone-based device is the vaginal contraceptive ring called the NuvaRing. This two-inch flexible ring, when placed in the vagina, releases progesterone and estrogen. It is very effective, resulting in only one or two pregnancies per 100.
Hormone Injection Perhaps the most effective of all forms of contraception is the hormone injection, Depo Provera, which is essentially a shot of progestin that interferes with ovulation. An injection is needed every three months. The side effects include irregular bleeding, weight gain, and headaches. But it is incredibly effective in preventing pregnancy, with fewer than one failure per 100.
IUD The intrauterine device is better known as the IUD, or the Coil. This method was very popular in the early 1970s and is still used in Europe today. The IUD is a copper T-shaped device inserted by a doctor inside the uterus to prevent the implantation of the egg. Unfortunately, it causes a lot of cramping and heavy bleeding. And in many cases this foreign body leads to the formation of pelvic inflammatory disease, and infection of the uterus and tubes that can cause infertility problems. An IUD is recommended only for women in monogamous relationships because the device acts as a highway for sexually transmitted diseases.
Plan B The only available post-coital contraception option is known as Plan B, or the morning after pill. Introduced in the late 1990s, this is an emergency contraception tool that must be taken within 72 hours of engaging in unprotected sex. It should not be used routinely because it involves taking pills with high quantities of progesterone, or progesterone with estrogen. The morning-after pill helps reduce the chance of a pregnancy by 80 percent for a single act of unprotected sex. But there are significant side effects involved, including nausea, vomiting and abdominal pain.
